No products in the cart.

Gastrointestinal Diseases: Symptoms and Treatment
Gastrointestinal Diseases: Symptoms and Treatment, Gastrointestinal (GI) diseases affect millions of people worldwide and can range from mild to severe. These diseases may arise from a variety of factors such as genetics, diet, lifestyle, infections, and autoimmune disorders. They can affect any part of the GI tract – from the mouth to the anus – and can cause a range of symptoms. In this article, we will discuss the most common GI diseases, their symptoms, and treatments.
1. Gastroesophageal reflux disease (GERD)
GERD occurs when the lower esophageal sphincter (LES) – a ring of muscle that separates the esophagus from the stomach – fails to close tightly. This allows stomach acid to flow back into the esophagus, causing irritation and inflammation. Symptoms of GERD include heartburn, acid regurgitation, chest pain, difficulty swallowing, and coughing. To treat GERD, doctors may prescribe antacids, proton pump inhibitors, or H2 blockers to decrease the amount of acid in the stomach, and make lifestyle changes such as avoiding trigger foods and maintaining a healthy weight.
GERD, resulting from the malfunctioning of the lower esophageal sphincter, can cause discomfort and interfere with daily life. However, with appropriate treatment and lifestyle modifications, individuals can effectively manage GERD symptoms and prevent complications. Medical interventions like antacids, PPIs, and H2 blockers play a significant role in reducing stomach acid and promoting healing. Coupled with lifestyle changes such as avoiding trigger foods and maintaining a healthy weight, individuals can achieve relief from GERD symptoms and improve their overall quality of life. It is essential to consult a healthcare professional for an accurate diagnosis and personalized treatment plan.
2. Peptic ulcer disease (PUD)
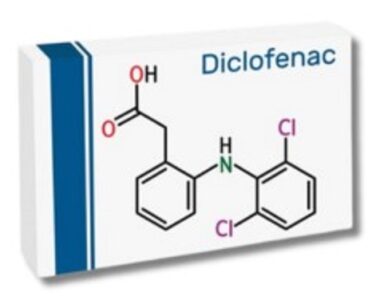
PUD refers to ulcers that develop in the stomach or upper small intestine. These ulcers can be caused by bacteria, including Helicobacter pylori (H. pylori), and chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs). Symptoms of PUD include abdominal pain, bloating, nausea, vomiting, and black or tarry stools. Treatment for PUD involves antibiotics to eliminate H. pylori, acid-reducing medications such as proton pump inhibitors (PPIs) and H2 blockers, and avoidance of NSAIDs.
3. Inflammatory bowel disease (IBD)
IBD refers to a group of chronic inflammatory conditions that affect the intestines. The two most common types of IBD are Crohn’s disease (CD) and ulcerative colitis (UC). Both CD and UC are characterized by inflammation that can affect any part of the GI tract. Symptoms of IBD include abdominal pain, diarrhea, rectal bleeding, weight loss, and fatigue. Treatment for IBD depends on the severity of the disease and may include immunosuppressive drugs, biologics, and surgery.
4. Irritable bowel syndrome (IBS)
IBS is a functional GI disorder that affects the colon or large intestine. It is characterized by a group of symptoms, including abdominal pain, bloating, constipation, and diarrhea. The cause of IBS is not well understood, although certain triggers such as stress, food intolerances, and hormonal changes may contribute to its development. Treatment for IBS may include lifestyle modifications, such as avoiding triggers and dietary changes, as well as medications to relieve symptoms.
5. Celiac disease
Celiac disease is an autoimmune disorder that affects the small intestine. It is triggered by gluten – a protein found in wheat, barley, and rye – and causes inflammation and damage to the small intestine. Symptoms of celiac disease include abdominal pain, bloating, diarrhea, weight loss, and fatigue. Treatment for celiac disease involves strict adherence to a gluten-free diet.
6. Diverticular disease
Diverticular disease refers to the formation of small pouches or sacs in the colon wall. These pouches, called diverticula, can become inflamed and cause symptoms such as abdominal pain, bloating, and changes in bowel habits. Diverticular disease can be managed through dietary modifications such as increasing fiber intake, as well as antibiotics and pain relievers.
7. Hemorrhoids
Hemorrhoids are swollen veins in the rectum or anus that can cause itching, pain, and bleeding. They can be caused by straining during bowel movements, pregnancy, and obesity. Treatment for hemorrhoids includes over-the-counter treatments such as creams and suppositories, as well as lifestyle changes such as increasing fiber intake and avoiding standing or sitting for long periods.
8. Gallbladder disease
This refers to conditions that affect the gallbladder, a small organ located under the liver. These disease can range from gallstones to cholecystitis, inflammation of the gallbladder. Symptoms of gallbladder disease include abdominal pain, nausea, vomiting, and fever. Treatment for gallbladder disease may include medications to manage symptoms, surgery to remove the gallbladder, or lifestyle modifications such as eating a low-fat diet.
9. Pancreatitis
Pancreatitis is inflammation of the pancreas, a gland located behind the stomach that produces digestive enzymes and hormones. Acute pancreatitis can be caused by gallstones or alcohol use, while chronic pancreatitis may result from conditions such as cystic fibrosis or long-term alcohol use. Symptoms of pancreatitis include abdominal pain, nausea, vomiting, and fever. Treatment for pancreatitis may involve hospitalization, pain management, and surgery in severe cases.
10. Hepatitis
Hepatitis refers to inflammation of the liver and can be caused by viral infections, autoimmune disorders, or drug or alcohol abuse. Symptoms of hepatitis include fatigue, abdominal pain, nausea, vomiting, and jaundice. Treatment for hepatitis will depend on the underlying cause and may include antiviral medications, immunosuppressants, or lifestyle changes such as avoiding alcohol.
Effective Strategies for Preventing GERD
Introduction:
Gastroesophageal reflux disease (GERD) is a chronic condition that can cause discomfort and disrupt daily life. While medications and lifestyle changes can help manage GERD symptoms, taking proactive steps to prevent its occurrence is equally important. This article discusses essential strategies for preventing GERD, emphasizing the significance of maintaining a healthy lifestyle, making dietary adjustments, and adopting proper eating habits.
Maintain a Healthy Weight:
Maintaining a healthy weight is crucial in preventing GERD. Excess weight, especially around the abdominal area, can increase pressure on the stomach and contribute to the weakening of the lower esophageal sphincter (LES). This can result in the backflow of stomach acid into the esophagus. Engaging in regular physical activity and following a balanced diet can help achieve and maintain a healthy weight, reducing the risk of GERD.
Watch Your Diet:
Certain foods and beverages are known to trigger or worsen GERD symptoms. To prevent the occurrence of GERD, it is important to identify and avoid these trigger foods. Common culprits include spicy and fatty foods, citrus fruits, tomatoes, chocolate, caffeine, alcohol, and carbonated beverages. Opting for a diet rich in whole grains, lean proteins, fruits, and vegetables can be beneficial in preventing GERD.
Eat Smaller, More Frequent Meals:
Consuming large meals can put pressure on the LES and increase the likelihood of acid reflux. To prevent GERD, it is advisable to eat smaller, more frequent meals throughout the day. This approach ensures that the stomach is not overly full, minimizing the chances of acid regurgitation into the esophagus. Additionally, taking the time to chew food thoroughly and eating slowly can aid in digestion and prevent the onset of GERD symptoms.
Avoid Eating Close to Bedtime:
Eating too close to bedtime can disrupt the digestive process and increase the likelihood of acid reflux during sleep. To prevent GERD, it is recommended to finish meals at least two to three hours before lying down. This allows sufficient time for the stomach to empty and reduces the chances of stomach acid flowing back into the esophagus. If necessary, elevating the head of the bed can further assist in preventing nighttime acid reflux.
Quit Smoking:
Smoking weakens the LES and can exacerbate GERD symptoms. If you smoke, quitting is highly recommended not only for preventing GERD but also for improving overall health. Consult with healthcare professionals or join smoking cessation programs for support in overcoming nicotine addiction.
Manage Stress:
Stress can contribute to various health issues, including GERD. Finding effective stress management techniques, such as engaging in regular exercise, practicing relaxation techniques like deep breathing or meditation, and seeking support from loved ones or professional therapists, can help reduce stress levels and prevent GERD symptoms.
In conclusion
GI diseases can affect anyone and can cause a range of symptoms that impact quality of life. However, with proper management and treatment, many GI diseases can be effectively controlled or even cured. If you experience any GI symptoms, it is important to consult your healthcare provider for an accurate diagnosis and treatment plan.



3,332 Comments