No products in the cart.

Is congenital heart failure fatal?
what is congenital heart Defect?

Is congenital heart failure fatal? Congenital heart disease mostly refers to a defect, which refers to one or more problems with the heart structure at birth. These abnormalities mostly occur when the heart or blood vessels don’t form correctly in utero.
Moreover, Congenital heart disease is a general term for a range of congenital disabilities that affect the normal way the heart works. The term “congenital” means the condition is present from birth. Congenital heart disease is one of the most common types of genetic disability. They can cause lifelong disability or death.
Congenital heart defects (CHDs) are present at birth and can affect the structure of a baby’s heart and how it works. They are the most common type of congenital disability. As medical care and treatment have advanced, infants with congenital heart defects live longer and healthier lives. Many now are living into adulthood.
Some Common Congenital heart Defects:
Following are the most common Congenital heart Defects:
Atrial Septal defect
Ventricular Septal defect
Aortic Coarctation
Disorder of the left side of the heart (hypoplastic left heart syndrome
Atresia of the trachea and/or bronchi
Fallot’s Tetralogy
The Completely Abnormal Venous Outflow from the Lungs
Agenesis of the Tricuspid Valve
Transposition of the Major Arteries (d)
Aortic Arch Truncation
Diastolic Heart Malfunction With Perforation of the Ventricular Septum
Atrioventricular septal defect
Critical congenital heart defects:
About 7,200 newborns in the United States each year are diagnosed with life-threatening congenital heart defects. Newborns with these cardiac problems often have trouble breathing, so it’s important to screen for them using pulse oximetry at least 24 hours after birth. The first year of life is a crucial time for treating severe congenital heart defect in infants. Critical congenital heart problems are the most severe type of heart defect, but there are many others that can be just as dangerous and may also necessitate treatment shortly after delivery.
Congestive Heart failure:
The heart may still be pumping blood despite cardiac failure. Instead, it indicates less effective cardiac function. Slower blood supply and higher intracardiac pressure can result from a number of different conditions and diseases. Therefore, the heart is unable to pump sufficient amounts of oxygen rich blood and nutrients to the body.
As a result, the heart’s chambers may either expand to accommodate more blood for pumping or stiffen and thicken. Although this aids in maintaining blood circulation, it may lead to a weakening of the heart muscle walls and an ultimate inability to pump blood effectively. In response, the kidneys could make you retain water and salt. Congestion can occur in various parts of the body if fluid accumulates there. This condition of heart called congestive heart failure. Only senior cardiologest treats Congestive heart failure.
How serious are most congenital disabilities?
Fortunately, not all cases of congenital heart disease in children require medical intervention. Children with other types of congenital cardiac abnormalities may need multiple procedures over several years.
Knowledge is power, and arming yourself with information on your child’s congenital heart problem will help you cope with the diagnosis and the years ahead.
How heart abnormalities are formed in the womb?
An infant’s heart begins to develop and beat throughout the first six weeks of pregnancy. At this pivotal stage, development also starts in the major blood arteries that supply and drain the heart.
Congenital cardiac abnormalities can manifest at this stage of a baby’s development. Genetics, specific medical disorders, specific drugs, and environmental or lifestyle factors like smoking are all possible contributors to the development of congenital disabilities, although the exact causes remain unknown.
Having a critical congenital cardiac defect is fatal:
Newborns with these heart abnormalities, which cause them to have low oxygen levels, can be detected by pulse oximetry screening at least 24 hours after birth. Critical congenital heart defect (CHD) babies require surgery or other operations during the first year of life. However, there are a variety of cardiac problems that, while not as life-threatening as major CHDs, may nonetheless necessitate treatment shortly after delivery. This illness is obviously fatal, and the death of your kid will result from any delay in detection and treatment.
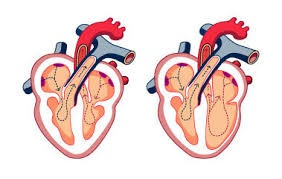
Does VSD can close as their Own?
Most VSDs close on their own or cause signs of congestive heart failure that may be treated surgically in time to save the patient’s life; therefore, they are not considered life-threatening. Serious arrhythmias occur in 16-31% of individuals with VSD, despite the generally benign clinical history of VSD. In a study with VSD and arrhythmias, one-third of all deaths in a cohort of medically managed patients were due to sudden cardiac death.
For all occurrences of VSD-related sudden death that have been documented in detail, cardiac hypertrophy has been identified as the underlying cause of death. We have seen four cases of infants as young as one-week old dying unexpectedly from VSD. Cardiomegaly was present in both cases, and in one, there was also a thickening of the media of the pulmonary arteries, with the smooth muscle extending into the small intralobular veins. The attending physician was sued for malpractice in 50% of our cases. We consider VSD to be a potentially fatal abnormality in newborns and young children and recommend close clinical monitoring.
High-output cardiac failure is a common complication of congenital abnormalities in children but not in adults. Cardiomyopathy and other forms of low-output heart failure affect some children. In about 8 out of every 1000 newborns, CHD is present. About 20% of individuals suffer from HF connected to CHD.
Adult congenital heart disease:
Condition(s) affecting the heart structure you are born with are collectively referred to as adult congenital heart defect (ACHD). Genetic disorders begin during fetal development and are visible at birth. These problems affect the heart’s ability to pump blood. Another term for these conditions is a congenital cardiac defect.
The severity of congenital cardiac defects can vary widely. Symptoms of cardiac illness might differ from person to person and from disease to disease, making diagnosis difficult until adulthood. For some, no symptoms are ever-present. Some people treated for these disorders as children continue to show symptoms as adults.
Treatment and diagnostic advancements have led to better results for those with ACHD. When diagnosed and treated in childhood, ACHD has a 90%+ survival rate into maturity. You will need ongoing medical attention to manage your disease properly if you are diagnosed with ACHD at any age, whether youth or adulthood.
Congenital heart defect diagnosis

An infant may receive a congenital heart defect (CHD) diagnosis before or shortly after delivery. However, other birth abnormalities are more subtle and we canot recognize until later in infancy or even later in life.
Studies for Diagnosis
Consistent visits to a cardiologist are essential if your child has a congenital heart problem. The cardiac specialist you see can do a battery of tests to diagnose your condition.
Your cardiologist will take a thorough medical history and conduct a physical examination during your scheduled appointment. A cardiologist can recommend chest X-ray, an electrocardiogram (EKG or ECG), or both. Patients undergoing Fontan procedures for cyanosis and single ventricle hearts should have regular blood tests.
A cardiology team member will explain each test’s results to you. Ask the doctor, nurse, sonographer, or technician any questions about what will happen. After all the tests are done, your cardiologist will review the results with you,realises risk factors and let you know whether further action is required.
It’s possible that further testing will be required if the results of the first round of exams don’t provide enough information for a definitive diagnosis. MRI, CT, Holter monitoring, stress testing, cardiac catheterization, and angiography.
Prenatal and pediatric diagnosis
In most cases, severe heart issues don’t appear until shortly after birth. Blue babies or extremely low blood pressure are just some of the issues affecting newborns. Problems with breathing, eating, or gaining weight result from other birth abnormalities.
Regular checkups are the best time to spot and treat minor health problems. Minor abnormalities rarely bring on symptoms. A child’s heart may murmur for various reasons, while the vast majority are perfectly normal.
Your child’s pediatrician or family doctor will likely recommend you to a pediatric cardiologist if they detect a cardiac condition based on symptoms or a heart murmur. Doctors specializing in pediatric cardiology are equipped to assess heart health and treat cardiac conditions in newborns, children, adolescents, and young adults. They have the resources to evaluate how often your child will require future heart exams and what tests and treatments your child will need.
Critical Congenital Heart Disease or Serious congenital heart defects:
Some birth abnormalities of the heart, known collectively as critical congenital heart disease (CCHD), manifest with immediate and potentially fatal symptoms and necessitate surgical repair within the first few months of life. If found early, CCHD is often curable. This umbrella includes both cardiac structural issues and rhythm disturbances. .
These issues might be quite minor (never necessitating heart surgery) or extremely serious (requiring multiple stages of open heart surgeries). Abnormal or missing heart chambers, holes in the heart, misplaced heart connections, and dysfunctional or abnormally tight squeezing are all possible manifestations of congenital cardiac defects. Most people with congenital heart disease don’t see a doctor until they are adults.
Can Peads who function normally at birth develop life threatning issues ?
Some infants with CCHD may appear and function normally at birth yet develop life-threatening issues just hours or days later. As per conditions of babies who are at risk for congenital heart defect (CCHD), a cardiologest identifies before they leave the nursery using pulse oximetry newborn screening, we can term this process as early detection.
This non-invasive technique detects the amount of oxygen in the blood. Infants with CCHD have a better chance of receiving treatment and living a normal life span if their health provider identifies, condition early.
The study of defect genesis
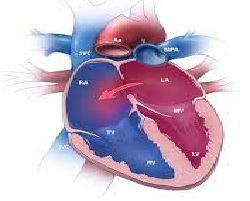
Reviewing the heart’s normal functions is a good first step in understanding congenital cardiac abnormalities.
The healthy circulatory system begins with the body, travels through the heart and lungs, then returns to the body via the lungs and the environment. The heart pumps blood to the lungs, receiving oxygen, and then pumps the blood back to the body.
Congenital abnormalities of the heart’s valves, chambers, arteries, and veins can cause disruptions to this circulation pattern.
The severity of congenital heart defects varies widely, from minor issues like “holes” between heart chambers to catastrophic anomalies like the lack of an entire heart chamber or valve.



887 Comments